The Road Less Traveled: A Journey to Bring Quality Improvement Training to a Pharmacy Residency Program
Kathlene DeGregory, PharmD, BCOP
Clinical Pharmacist, Stem Cell Transplant – UVA Health
Charlottesville, Virginia
Amy L. Morris, PharmD
Scientific Director of Oncology
Pharmacy Times Continuing Education
Choosing A Path
Since the time of the publication “To Err is Human: Building a Safer Health System“1 in 2000, healthcare has begun to shift focus to examine the systems we use to provide care and improvement of those systems. In 2001 the Institute of Medicine published “Crossing the Quality Chasm”2 to further describe how faulty system design and system performance are primary root causes for problems affecting patient safety, as well as how frontline staff are in key positions to affect change to those systems.3 At the University of Virginia (UVA), oncology pharmacists embarked on a journey to improve those systems and to educate others on the use of Quality Improvement (QI) tools.
The American Society of Clinical Oncology (ASCO) offers a quality-training program (QTP) to teach busy oncology clinicians how to improve the systems in which they work. ASCO QTP is a 6 month workshop designed to help interdisciplinary oncology teams develop, implement, and assess quality improvement changes within their organization. During the program, teams learn quality methodology, tools, and sustainability design as well as learning about teamwork, communication, and high reliability organizations. Three UVA oncology pharmacists, including the authors, attended ASCO QTP as part of interdisciplinary teams executing QI projects within the hematology/oncology service line. Final outcomes of UVA projects included reduction in length of stay and reduction in time to treatment of oncology patients. Due to the success of the UVA teams in executing QI initiatives, UVA hospital leadership approved tuition reimbursement to support additional employees attending the QTP program. We began to apply the tools and principles of QI into our daily practice, and as the value of this training became more apparent, we recognized the impact and importance of educating our fellow pharmacists as well as our pharmacy residents. The PGY2 oncology residency program began including their PGY2 resident as a team member in projects going through ASCO QTP but were unable to send the resident to the full training due to cost and timing of the program. So how does UVA ensure that our residents receive training in these valuable skills? Two oncology pharmacists decided we would just have to provide the training ourselves! In the fall of 2020, we embarked on a journey to bring this idea to fruition.
Into The Woods
Prior to 2020, all PGY1 and PGY2 residents at UVA were required to complete a quality improvement project (QIP) per ASHP standard Goal R2.2: “Demonstrate ability to conduct a quality improvement or research project in the advanced practice area”, but the QIP was often structured like a Medication Use Evaluation (MUE) or a research-style project with a quality outcome as the primary end point. Published QI tools were not utilized in an official capacity for these projects, and we were especially cognizant that R2.2.3 addressing data evaluation and sustainability could be improved by using validated quality analysis tools via continuous improvement cycles. We presented a proposal to the Residency Oversight Committee at UVA to restructure the content of QIPs, narrowing our scope to focus on the PGY1 program. We also included the PGY2 oncology resident due to our close involvement with the PGY2 oncology program. We developed a structure for education similar to what we had experienced in our own quality training via ASCO. This included conducting a QIP over six months using The Model for Improvement as a backbone and incorporating the Plan-Do-Study-Act (PDSA) cycle. In terms of our qualifications for leading this effort, each of us had completed the ASCO QTP, institution specific LEAN training, as well as online QI modules provided by the Institute for Healthcare Improvement (IHI) open school. We designed our own training materials based on experiences with these organizations and review of the quality literature. To kick off, we conducted a preceptor development session outlining the new structure and the tools we would be using. All preceptors of PGY1 residents were asked to attend. We developed three, 1-hour didactic teaching sessions for the residents given at various intervals throughout the project timeline. We decided to serve as coaches for all projects to provide “in the moment teaching” as well as guidance and support for a new process for both residents and preceptors. The tools taught and utilized included process mapping, affinity sort, cause and effect diagramming, Pareto charts, priority matrix and statistical process control (SPC) charts. The projects were presented as posters at the Vizient meeting held in conjunction with the American Society of Health-System Pharmacists (ASHP) Mid-Year meeting.
Seeing The Forest for The Trees
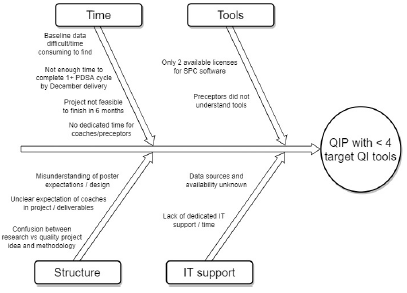
In our inaugural year, 6 PGY1 projects were completed. Of these, only 2 projects completed a full PDSA cycle within the 6-month time frame. Only 1 project included our target 4 QIP elements: Problem/aim statement, use of diagnostic tools (e.g., Pareto charts), analytical tools (e.g., statistical process control charts), and completion of 1 full PDSA cycle. The mean was 1.8 QI elements completed per project. In the true spirit of process improvement, we brainstormed potential barriers (Figure 1). The biggest areas for improvement revolved around time to educate both residents and preceptors on QI and time for residents to conduct the project.
Figure 1: Fishbone Diagram: Year 1 Quality Improvement Project
Changing Course
After brainstorming solutions to our identified barriers and prioritizing what was feasible and within our scope as preceptors, we made significant modifications to the QIP. Our QI committee joined with the existing research committee to create a longitudinal project committee. PGY1 residents chose either a research project or a QIP, both yearlong. Residents would attend all didactic teaching or presentation sessions for research and quality regardless of their project type, as both projects were equally important to our residency curriculum. Didactic sessions were updated annually based on previous resident feedback, including more detailed discussion on the use of diagnostic and analytical tools. In addition, a representative from the pharmacy informatics and technology (IT) team attended project proposal sessions to provide guidance on how to efficiently find baseline data. In order to spread the workload, we began training several preceptors to serve as coaches in the future, as coaching multiple QI projects during the first years was a significant workload increase for us. Due to some confusion over involvement of the QIP coach, we defined the role of the QIP coach in guidance documents provided to the residents at the beginning of the year. Expectations included the following: the QIP coach should be included in early meetings, should have regular updates regarding milestones for poster and platform presentations, and should review final posters and presentations for accuracy. An online resource folder with tip sheets for using QI tools and additional examples of posters and manuscripts was created. Unfortunately, finding dedicated precepting/coaching time was not something that could be implemented at this time.
In year 2, a total of 8 quality projects were selected by PGY1 residents. Quality coaches were assigned to each project to help guide each team and continue the “in the moment” teaching and expand upon the didactic teaching. All PGY2 residents were encouraged to use the PGY1 process and presentation forums, but it was only required for the PGY2 oncology resident. Residents presented their problem and aim statements and some of their diagnostic work in a group setting for shared learnings between all teams. Residents presented preliminary information in a poster format at ASHP Vizient in December, a platform presentation at University of North Carolina Research in Education and Practice Symposium (UNC REPS) in May, and a manuscript suitable for publication in June.
Into The Clearing
In our second year, 4 projects included all 4 target elements and we improved to a mean of 3.5 elements included per project. In addition to the improvement in using QI tools, 2 projects received special recognition. The PGY1 project entitled “Assessing Medication Access Barriers in Patients Living with HIV” received the top prize for the UVA Young Investigator Research Award and was invited for poster presentation at the 2022 National Ryan White Conference on HIV care and treatment. The PGY2 oncology project entitled “Utilization of UVA Health Pharmacies for Outpatient Prescription Dispensation in the Malignant Hematology and Thoracic Oncology Clinics” was awarded with a Quality Research Certificate at the 2022 HOPA Annual Conference.
Barriers identified from resident, preceptor and coaching feedback included ongoing preceptor confusion over how a research project was distinctly different from a QI project, as well lack of clarity in expectations for presenting QI tools in a poster format and a platform presentation. Time taken to obtain baseline data meant several teams suffered early delays in identifying outcome measures and implementing countermeasures.
The Steep Climb
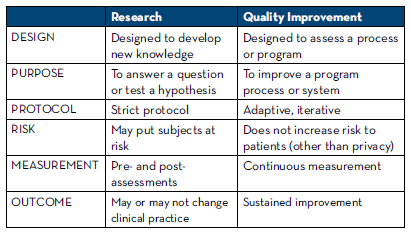
Based on year 2 feedback, our focus for improvement the current year involves investing in training for our preceptors in the use of QIP tools using existing educational avenues in order to free up coaching time and make precepting time more efficient. UVA Health was eligible to purchase an educational group subscription to IHI open school. The longitudinal project committee created two preceptor development tracks, one for research and one for QIP. Preceptors on the QIP track will complete the 5 online QI modules from IHI, as well as attend the in-house sessions. Additional focus will be on contrasting elements of QI with those of research to help preceptors and residents become comfortable with the distinction between them; Table 1 was included as part of this work.
The importance of accurate and relevant baseline data cannot be overstated. Ongoing discussions with IT leaders for assistance in obtaining baseline data in a timely manner are continuing. A mantra from QTP is “fail forward,” meaning learn from mistakes and failures to improve upon the system; one example included re-evaluating our own internal “measure” of success. Even though some projects from the previous year didn’t contain all four target elements, there was great value in the work the teams completed and those learnings were important to share. For example, the PGY2 oncology project focused on obtaining and understanding accurate baseline data, such that an improvement project could begin. Another team realized during the analysis of their diagnostic data that there were flaws in the process map and the process measure, revealing the team did not have a full understanding of the root problem and therefore they could not develop effective countermeasures. Rather than abandoning the work, they used this as an opportunity to illustrate the importance of working together as a team to understand the process as it currently exists, not a perceived ideal state.
Table 1: Distinguishing a Research vs Quality Improvement Project
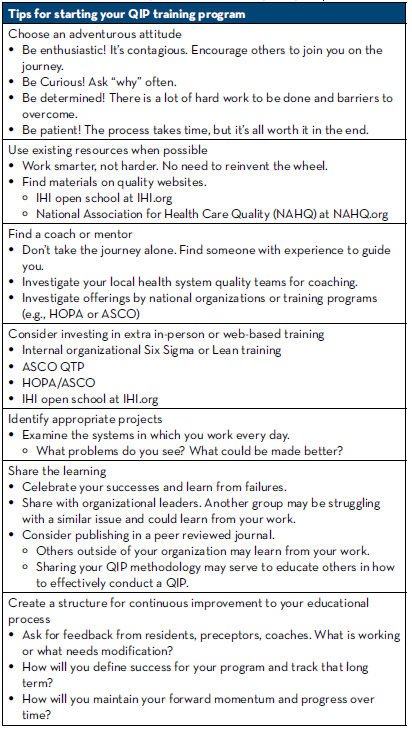
The Map And Compass
While our journey to educate pharmacy residents in the art of QIP is just getting started, we certainly have education to share regarding what it takes to start a program similar to this (Table 2).
Table 2: Tips for Starting Your QIP Training Program
As we continue to develop and improve our QIP program via PDSA cycles, we continue to look for external opportunities to grow as well as share our work. Our PGY2 oncology resident is currently attending the 6 month ASCO QTP / HOPA collaboration course, the first UVA resident to be funded to attend the program. We also relished the opportunity to write this newsletter and share our experience with those who may have started the journey or are wanting to take first steps but don’t know where to start. The road less traveled is full of surprises and difficult terrain, but the rewards and benefits are worth every step. Together we can change the face of health care, one process improvement at a time.
REFERENCES
- Institute of Medicine (US) Committee on Quality of Health Care in America. To Err is Human: Building a Safer Health System. Kohn LT, Corrigan JM, Donaldson MS, editors. Washington (DC): National Academies Press (US); 2000. PMID: 25077248.
- Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: The National Academies Press. https://doi.org/10.17226/10027.
- Institute of Medicine (US) Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine. The Future of Nursing: Leading Change, Advancing Health. Washington (DC): National Academies Press (US); 2011. PMID: 24983041.
- Al-Surimi K. Research versus Quality Improvement in Healthcare. Glob J Qual Saf Healthc. 2018;1(2): 25–27.
- Casarett D, Karlawish JHT, Sugarman J. Determining When Quality Improvement Initiatives Should Be Considered Research: Proposed Criteria and Potential Implications. JAMA. 2000;283(17):2275–2280.
- Langley GL, Moen R, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance (2nd edition). San Francisco: Jossey-Bass Publishers; 2009.
- How to Improve. Institute for Healthcare Improvement. http://www.ihi.org/resources/Pages/HowtoImprove/default.aspx
