Integration of a Specialty Pharmacy Team within Oncology Care
Kristina Lo, PharmD, BCOP
Senior Clinical Pharmacist, Oncology Specialty Pharmacy
UC Davis Health
Sacramento, CA
Iris C. Zhao, PharmD, BCPS, BCOP, APh
Senior Clinical Pharmacist, Oncology Specialty Pharmacy
UC Davis Health
Sacramento, CA
Introduction
Oral oncolytic development has been increasing steadily, making up about 25-35% of the new oncology drug pipeline.1 With this shift towards oral oncolytic use, many parts of the healthcare system need to evolve to match the pace of this change. While physicians, allied health professionals, and other medical personnel try to keep up with these changes, one of the greatest challenges that plague healthcare systems is staff shortages across all disciplines.2 Timely care, medication education, and medication access are just a few of the many things that can be negatively affected by staff shortages, potentially leading to poorer clinical outcomes.3 To help bridge these gaps, we developed the Oncology Specialty Pharmacy (OSP) at UC Davis in the adult hematology/oncology clinic setting with a focus on oral oncolytics.
Initial Integration into the Hematology/Oncology Clinic
Our OSP started as an initial year-long pilot in 2013 with one pharmacist providing telephone calls to patients one day a week to monitor adherence and toxicities. In September 2014, 1 full-time employee (FTE) pharmacist and 1 FTE technician were introduced into the adult hematology/oncology clinic setting to work directly with our multi-disciplinary staff. Since then, we have expanded to 4 FTE pharmacists and 4 FTE technicians over the last 7 years.
The OSP and clinic are staffed by clinical pharmacists with appropriate experience and training, such as completion of a PGY1 Pharmacy Residency Program with an emphasis in Oncology and/or a PGY2 Oncology Pharmacy Residency Program, or equivalent (e.g., Board Certified Oncology Pharmacist). Experience with the hematology/oncology patient population and demonstrated competence in cancer therapy and supportive care medication management are necessary for pharmacists prior to involvement in the OSP.
There is no specific requirement for technicians who staff the OSP and clinic, though experience with financial assistance and prior authorizations (PAs) is preferred. Currently at UC Davis all technicians have at least 5 years of experience in various settings from retail and/or specialty settings. The pharmacy team plays a pivotal role in relieving significant burden from patients experiencing the financial toxicities of their therapies through applying for financial assistance on behalf of the patient. In addition, having dedicated pharmacy technicians to submit PAs can decrease the time to initiation of therapy.
Clinical Pharmacy Services – A Hybrid Model
Outpatient pharmacy service models across the nation vary in the degree of integration into the clinic setting. Traditionally, specialty pharmacies have limited or no affiliation with the patient’s practice-based oncology care team. This can lead to significant logistical barriers to oncology care including a lack of shared health records for medical communication and documentation.4
The integrated OSP service at UC Davis allows the oncology pharmacists and technicians a unique opportunity to serve as both a tele-provider to patients via phone-based services and on-site support to providers and patients in the clinic. While our initial pilot program only monitored adherence and toxicities, our list of services was later expanded to meet the most critical needs for our patients once full-time staff were integrated into the clinic space in 2014. Currently, the OSP team provides a full spectrum of services, including clinical evaluation of therapy, PA support, financial assistance, patient and caregiver education, regular lab monitoring, drug/herb interaction evaluation, and supportive care management.
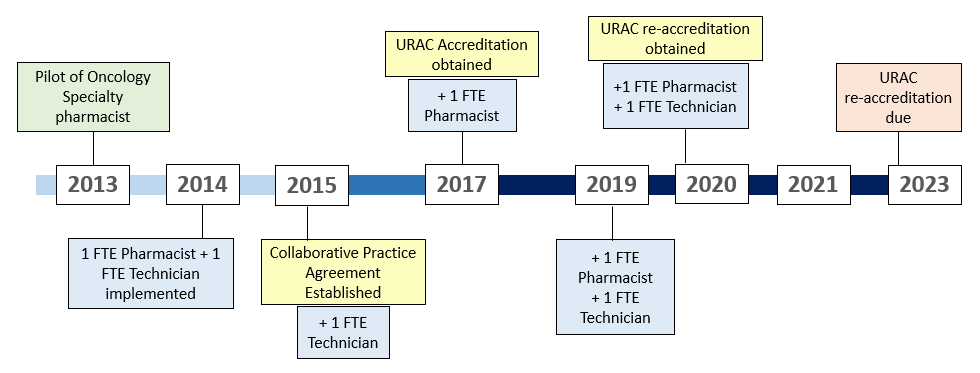
Figure 1: Timeline of the UC Davis Oncology Specialty Pharmacy

Figure 2: Overview of Oncology Specialty Pharmacy workflow
Initial Prescription of Therapy
Oncology specialty pharmacists play a key role in the discussion of the appropriateness of a therapy and collaborate with providers in determining a dosing and monitoring plan. Once a treatment plan with an oral oncolytic has been established, providers send prescriptions directly to the on-site dispensing pharmacy. The dispensing pharmacy staff are trained to communicate directly with the OSP team in the benefits investigation process and triage prescriptions to dedicated PA oncology technicians who submit PA’s for all cancer center prescriptions. Once the PA process is complete, OSP technicians evaluate prescription copays and drive the patient assistance process for prescriptions with high copays. Patients who are referred to the OSP are added to a confidential list of patients to be educated and monitored by the oncology specialty pharmacists.
Education
In order to make informed decisions about treatment, patients and caregivers must receive education on administration and monitoring of the oral oncolytic, expected outcomes, adverse effects, and costs of therapy.5 Specialty pharmacists provide comprehensive medication education and a full medication reconciliation to all patients who are initiated on an oral oncolytic and ensure pertinent baseline laboratory testing is completed prior to initiation of therapy, if applicable. These actions can be completed over the phone, in-clinic at the time of prescription, or at the dispensing pharmacy at time of dispense.
Clinically Meaningful Management and Follow-up
Once patients initiate therapy, pharmacists follow a standardized monthly interval for pharmacist follow up. Lab tests and recent scans are evaluated to determine continued appropriateness of therapy; patients are assessed for correct administration of medication, adherence, and adverse events; and refills are processed and arranged for pick up or delivery. Evaluation and adjustment of monitoring plans, clinic visits, and/or prescription of additional supportive care prescriptions are also performed at this time. More frequent follow up is implemented for patients that are determined to be at high-risk for non-adherence or adverse events.
Current practice at UC Davis is to conduct education for all patients prescribed an oral oncolytic, whereas regular follow up calls are conducted for patients whose specialty medications are filled at the UC Davis dispensing pharmacy, instead of an external specialty pharmacy. All patients, regardless of their filling pharmacy, are educated to call the OSP team for questions or assistance with adverse event management.
Patient and Provider Impact
To evaluate current practices and services, patients and providers are sent satisfaction surveys to evaluate their interactions with the OSP team. Surveys are created by the National Association of Specialty Pharmacy (NASP) and distributed through either direct mail or web-based options quarterly. These survey results provide the OSP team insight into ways to develop and improve services.
Adherence data
In addition to patient and provider satisfaction, the most important detail is improved patient care and outcomes. While clinical outcomes may be difficult to ascertain, patient adherence is necessary to optimize their chance for a successful outcome. In 2015, a retrospective analysis was performed to evaluate adherence of our OSP and it was observed that our program was able to significantly improve patient adherence.6 Adherence was analyzed through medication possession ratio (MPR).
Challenges and Limitations
Given the recent growth in the use of oral oncolytics and their high-cost nature, more payors are setting limitations and/or mandating which pharmacies a covered patient can receive their specialty medications from. In addition, manufacturers are narrowing the distribution of their specialty medications to certain pharmacies to reduce distribution costs, among other reasons. Payor lockouts and limited distribution models limit the specialty pharmacists’ assessment of adherence and lead to delays in treatment initiation or continuation.7 In order to offset this challenge, the UC Davis OSP team implemented the pharmacy technician service of contacting external specialty pharmacies to follow up on prescriptions rerouted outside of the health system.
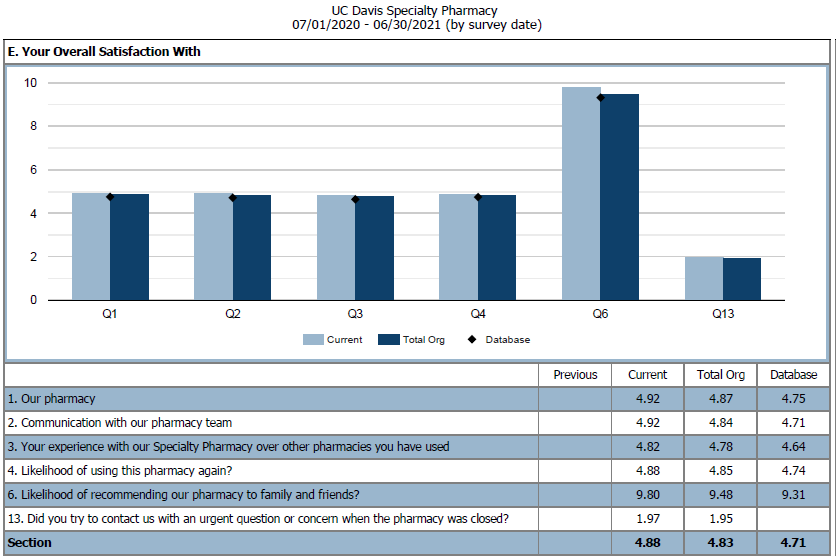
Figure 3: NASP Patient Overall Satisfaction Survey from July 2020 - 2021. We compared UC Davis Oncology Specialty Pharmacy to other UC Davis specialty programs and the NASP database.
Generalized growth in cancer care and use of oral oncolytics has led to an increased need for additional OSP staff which has been challenging to meet from a hiring perspective. Growth in the specialty pharmacy team as well as staff in other interdisciplinary areas had led to a shortage in available clinic space which is critical to continued on-site pharmacist support.
Agreeing upon a single case management program has also been a challenge for the UC Davis OSP. Although there are case management programs available, most programs do not interface with the health systems’ electronic medical record (EMR) which leads to increased time spent on duplicate documentation.
A continual workflow challenge for the OSP team has been ensuring that our practices meet the standards efficiently and thoroughly for multiple accrediting bodies. The UC Davis Cancer Center has been American Society of Clinical Oncology (ASCO) Quality Oncology Practice Initiative (QOPI) certified since 2016 and our specialty pharmacy has been Utilization Review Accreditation Commission (URAC) accredited since March 2017. With both of these accrediting bodies requiring different information, follow-up frequency and documentation are tailored to meet the varying standards from both QOPI and URAC.
Future Directions
There is a continued need for pharmacist outreach to encourage patient adherence to medications and manage supportive care to overcome the clinical implications of payor lockouts and limited distribution models. A primary goal of the UC Davis OSP is to have regular pharmacist outreach for all patients regardless of their filling pharmacy.
The increased use of oral oncolytics and the paralleling growth in challenges provide a glimpse at future opportunities for oncology pharmacists. Currently at UC Davis, specialty pharmacists are caring for any diagnoses and their associated oral therapies. However, there is the potential for pharmacists to become disease state specific which may provide more consistency for providers, nursing, and patients.
Another consideration for the future includes transitioning oral oncolytic orders to EMR oncology treatment modules leading to a more pharmacist-driven prescription process. Challenges include adjusting the specialty pharmacy workflow, provider buy-in and training, and additional information technology (IT) and pharmacist support. Additional IT and pharmacist support is critical as there are numerous oral therapies and their associated monitoring needs are unique to each individual medication.
Conclusion
The oncology pharmacist is a commonly untapped resource that can be utilized to help bridge many gaps that exist in our current healthcare situation. While OSP is simply one way to better optimize the oncology pharmacy staff, this is certainly not without its own challenges. Resources continue to be scarce, with drug and staff shortages rampant worldwide. Despite this, we have shown that OSPs can continue to be an opportunity for institutions to provide the desperately needed relief for both patients and medical staff, while providing the recognition that the pharmacy team can provide so much more than traditionally thought.
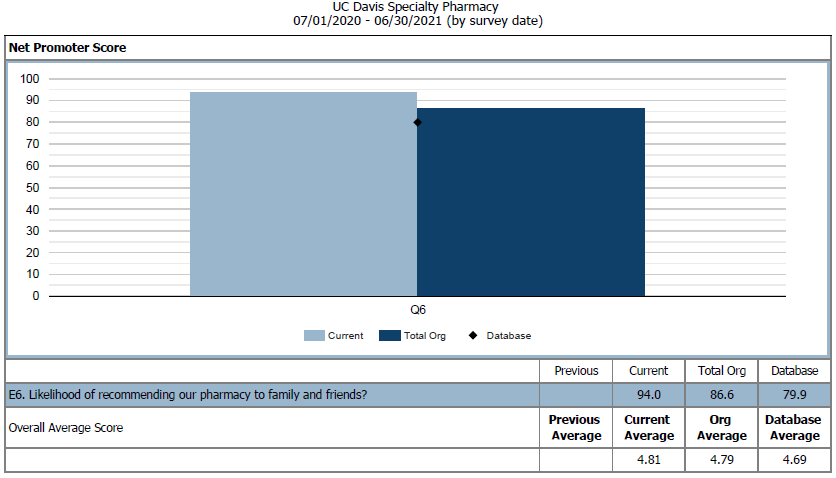
Figure 4: NASP Provider Net Promoter Score for Q6 in 2020 – 2021. We compared UC Davis Oncology Specialty Pharmacy to other UC Davis specialty programs and the NASP database.
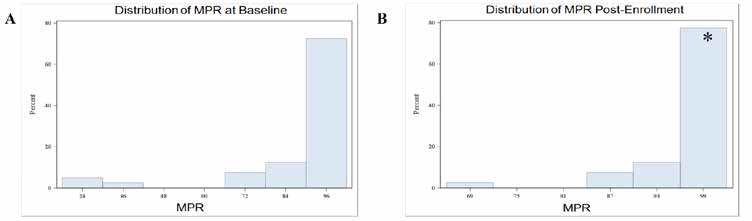
Figure 5: OSP Adherence Analysis from 2013-2014. A. MPR Analysis at Baseline. Mean MPR at baseline was 90.3%. B. MPR Analysis Post-Enrollment into our OSP. Mean MPR post-enrollment was 99.3%. *Mean increase = 9.08% (P=0.02).
REFERENCES
- Stokes M, Reyes C, Xia Y, Alas V, Goertz HP, Boulanger L. Impact of pharmacy channel on adherence to oral oncolytics. BMC Health Serv Res. 2017;17(1):414. doi:10.1186/s12913-017-2373-2
- Solutions to the Oncology Workforce Shortage. Ensuring Quality Cancer Care through the Oncology Workforce: Sustaining Care in the 21st Century: Workshop Summary. Institute of Medicine (US) National Cancer Policy Forum. Washington (DC): National Academies Press (US); 2009. (https://www.ncbi.nlm.nih.gov/books/NBK215257/)
- Lafferty, M et al. Causes and Consequences of Chemotherapy Delays in Ambulatory Oncology Practices: A Multisite Qualitative Study. ONF. 2020, 47(4), 417-427
- Muluneh B, Schneider M, Faso A, Amerine L, Daniels R, Crisp B, et al. Improved Adherence Rates and Clinical Outcomes of an Integrated, Closed-Loop, Pharmacist-Led, Oral Chemotherapy Management Program. J Oncol Pract. 2018 Jun;14(6): e324-e334. doi: 10.1200/JOP.17.00039
- Mackler E, Segal E, Muluneh B, Jeffers K, Carmichael J. 2018 Hematology/ Oncology Pharmacist Association Best Practices for the Management of Oral Oncolytic Therapy: Pharmacy Practice Standard. J Oncol Pract. 2019 Apr;15(4):e346-e355. doi: 10.1200/JOP.18.00581
- Chen Zhao I, Lai J, Seiki B, Wilson M, Brennan L, Li T, Wun T. Evaluation of a pharmacist-driven oral chemotherapy adherence program. Journal of Clinical Oncology. 2015. 33:15_suppl, 6569-6569
- Savage S, Bates J, Muluneh B. Challenges Continue for True Patient- Centered Access. Specialty Pharmacy Times. 2016 June; 7(3)
